So, what is asthma?
Introduction
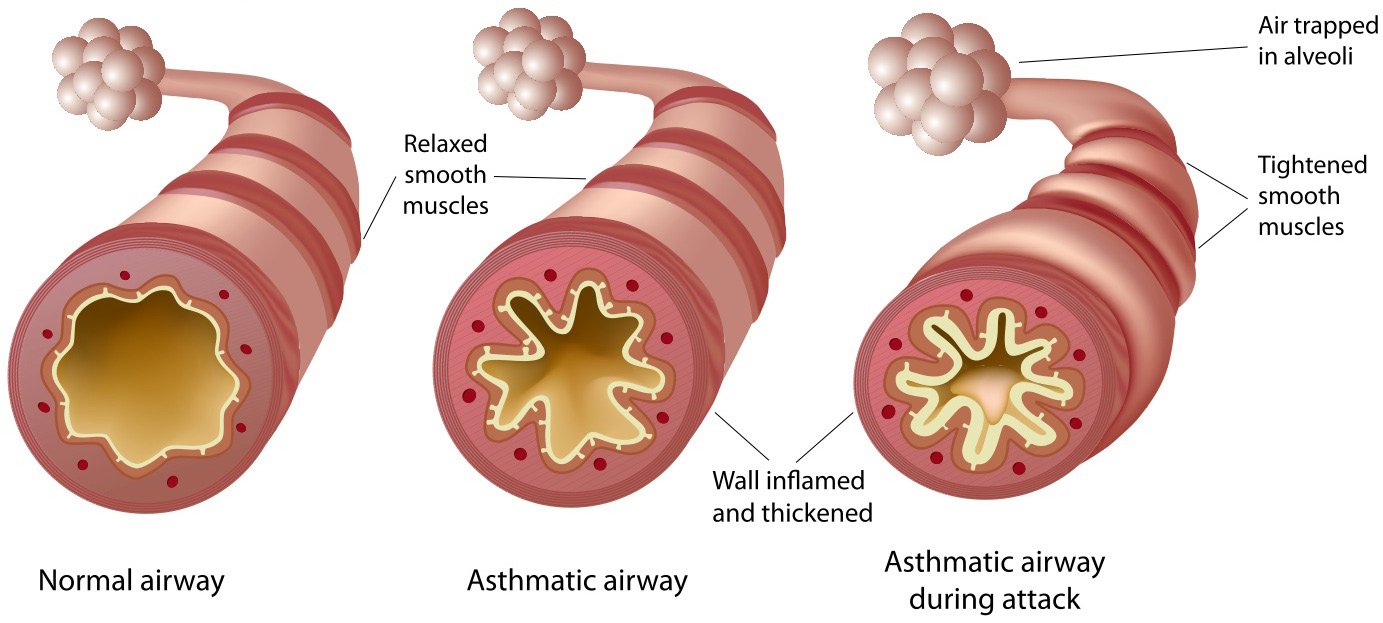
Asthma is a chronic lung disease that affects many children and adults across the world. The disease is characterized by narrowing of the small airways in the lungs due to muscle tightening, soft tissue swelling, and increased mucus production in the airways.
All of this makes it harder for your child to breathe, especially when they are trying to let their breath out. This can cause the lungs to become over filled with air (hyperinflation), which makes it even harder to breathe.
Asthma is a disease that can create daily symptoms, however, it is most commonly recognized during an asthma attack, which is a sudden worsening of symptoms due to a trigger.
Common triggers for childhood asthma include:
Viruses, like the common cold or influenza (the most common trigger)
Allergies, if your child is allergic to something like dust or animals
Cigarette smoke and pollution, is an extremely important trigger to avoid
Mold, the black stuff you may see in basements or bathrooms
Cold Air, keep an eye out for coughing that worsens when they go outside
Exercise, may bring out coughing and wheezing out of proportion to other children
Strong Emotions, like laughing or crying
Please see the video below for a more detailed explanation, before reading on!
Medications
While asthma is a chronic condition, there are safe medications that, when used correctly, are able to achieve asthma control in the vast majority of children. There are three main components of treatment for asthma:
Trigger Avoidance - the most important treatment; if you know what your triggers are, and can avoid it, do so! Sometimes, this means asking a parent to quit smoking, or making the difficult decision to get rid of a family pet if the child is allergic.
Relievers - medications like salbutamol or Ventolin, the ‘blue puffer’ act quickly to relax the tight muscles in the airway and give some relief of symptoms. This medication does not last long and without addressing the underlying problem, will not lead to asthma control.
Controllers - most commonly inhaled corticosteroids (ICS), such as fluticasone/Flovent/the ‘orange puffer’ or ciclesonide/Alvesco/the ‘red puffer’. These medications treat the underlying inflammation that makes muscles tighten, airways narrowed, and filled with mucus. There are many other medications that also function as controllers that may be necessary based on your child’s specific needs and your doctor’s assessment. It is important that controller medications be taken every day. Sometimes, during an asthma attack, oral corticosteroids (OCS) need to be used, which leads to a much larger systemic exposure to steroids than ICS. This exposure is usually necessary in an emergency.
One way to contrast Relievers and Controllers is to compare symptoms (and their treatment) to problems (and their treatment). Think of an ear infection (problem) with a fever (symptom), Tylenol will help bring down the fever but won’t treat the problem, which needs antibiotics. In asthma, the controller treats the problem and makes us less likely to need a reliever! It is therefore important that reliever medications only be used for symptoms, and that if they are used frequently, a controller medication be used as well.
One final component of reaching good asthma control is medication technique. Taking a puffer is often made to look very easy in movies and television. For this reason, typical puffers should ALWAYS be used with an Aerochamber/spacer device. Be sure to check with your doctor or healthcare provider that you are giving your child’s medications correctly. For additional support, please also see the videos below:
Achieving Control
For those children who are controlled, it should be very difficult for someone to know they have asthma (because their symptoms, if any, should be very mild)!
The definition of asthma control is:
No symptoms, or need for relievers at night (your child’s asthma should not impact sleep)
Limited symptoms, or need for relievers during the day (<3 times per week)
Ability to attend school and participate in physical activity without limitation
Any increase in symptoms (such as an attack due to a trigger) should be mild and short-lived (only a few days) and not requiring oral steroids.
Finally, many children will eventually outgrow their childhood asthma. You will talk with your doctor about when might be a reasonable time to stop controller medications to see if your child needs them any longer. This will always be a discussion of risks versus benefits, as asthma attacks can be very dangerous, even causing death.
Together, you and your doctor can chart a course for achieving asthma control in your child, so that they can live the full, and active life you wish for them!
For more great information, check out SickKids’ AboutKidsHealth Asthma Learning Hub!